Population health management (PHM) is moving forward at a very rapid pace, due to the shift in healthcare priorities and related business models coupled with the ever increasing cost of healthcare and helped by the emergence and utilization of big data analytics.
Before we get to the issue of how population health management works, we first need to understand what population health is. Defined as, “the health outcomes of a group of individuals, including the distribution of such outcomes within the group”, population health aims at reducing health inequities and disparities among different population groups, due to factors like the social determinants of health (SDOH).
What is population health management?
A method to improve population health and defined as, “the technical field of endeavor which utilizes a variety of individual, organizational and cultural interventions to help improve the morbidity patterns (i.e., the illness and injury burden) and the health care use behavior of defined populations”, population health management differs from disease management. It includes more chronic conditions and diseases, uses a single point of contact and coordination and works with predictive modeling across multiple clinical conditions. PHM also includes intensive care management for those at high risk levels and personal health management for those at a lower health risk level.
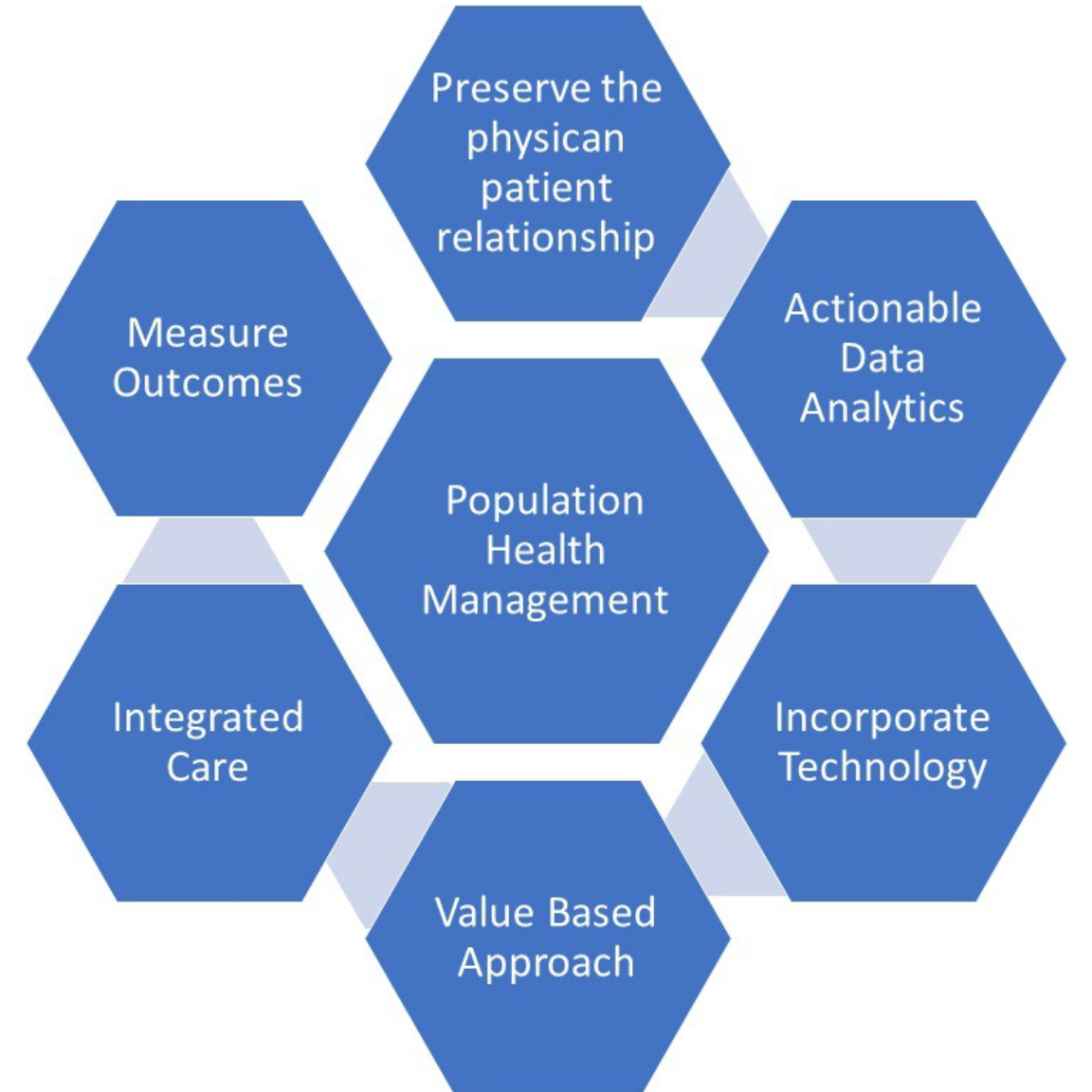
Population health management works by aggregating patient data across multiple health information technology resources, analyzing the collected data into a single record, and initiating actions through which healthcare providers can improve the clinical and financial outcome for the patients.
Population health management thus provides a comprehensive and authoritative strategy to create policies and improve the systems that effect quality, access and outcome of health care, ultimately leading to an improvement of the health of the entire population.
What are the key benefits of PHM?
Population health management has advantages for everyone associated with healthcare – from the patient, to the healthcare provider; from the society to the government. Listed below are some of the key advantages of population health management.
- Better health outcomes: The goal of PHM is very simple – reducing costs of healthcare while improving the quality of healthcare services.
- Preventing and managing diseases: Using data and IT solutions, PHM works to improve the care of those with chronic diseases. Keeping track of and managing such patients effectively reduces the costs involved. Analyzing collected data also ensures the readiness of healthcare providers towards any epidemic outbreaks, resulting in efficient and effective counter measures, which in turn reduces the costs for both the patient and the healthcare system.
- Closing the gaps in healthcare: Using a business intelligence tool to aggregate data, which provides a complete clinical picture of the patient, PHM closes the gaps in healthcare providing by allowing all concerned with real time access to monitor, track and address patient needs. Incorporating the EHR, laboratory records, prescription data, billing records and insurance data, healthcare providers can trace out required needs and gaps in either the data or the service delivery.
- Financial benefits for patient and provider alike: Using existing data would help early detection of problems, thus resulting in preventive treatment, which could be less expensive for the patient. Tracking and monitoring the patients ensures regular visits to the health provider, which in turns brings repeat business to the practice. Using PHM results in improved clinical outcome and reduced costs – a win-win situation for everyone.
Challenges facing population health management
PHM is the biggest idea in healthcare this year and is likely to become a US$ 30 billion industry by 2020. However, population health is a multidisciplinary concept with public health agencies, social institutions, policymakers, healthcare providers and patients, all having a stake in it. Making sure that the system functions smoothly and efficiently will require many challenges to be addressed and overcome.
The biggest challenge for healthcare providers is to transform the national infrastructure from a volume based to a value based model, with a goal to provide higher quality healthcare at a lower cost, while expanding access to their services.
Some of the other challenges that need to be addressed are:
- Shortage of managers in population health expertise.
- Quantifying population health – to avoid oversimplifying problems or overinvesting in solutions.
- Adhering to Regulatory demands.
- Managing infection prevention and control.
- Consolidation amongst all the stake holders in PHM.
- Integrating existing systems with PHM effectively.
- Overspecialization of the physician workforce creating shortage of primary healthcare physicians.
- Urban concentration of healthcare at the cost of rural areas.
- Differences in reimbursement rates.
- Making sense of the large volumes of data and integrating it for optimum use.
Population health management can work wonders for a country. With healthier people through preventive care, the potential to live longer, produce more based on the work done, increase individual earnings will positively improve the economy of the country.