The new MACRA implementation has brought about nothing but chaos and confusion among medical practitioners, and more so for cardiovascular specialists.
What is MIPS and what is MIPS Medicare?
MIPS (Merit Based Incentive Payment System) is the new payment model that is geared towards a value-based payment rather than the existing service based model.
This shift comes with a number of changes that a medical practitioner has to incorporate into his/her practice in order to ensure that the revenue is not amiss.
As you will see in this article, cardiologists need to understand MIPS architecture and MIPS reporting lest the lack of knowledge harm their careers or reputation.
What Does MIPS Stand for in Healthcare?
Now that we know what MIPS is, we need to answer the question: What is MIPS in healthcare?
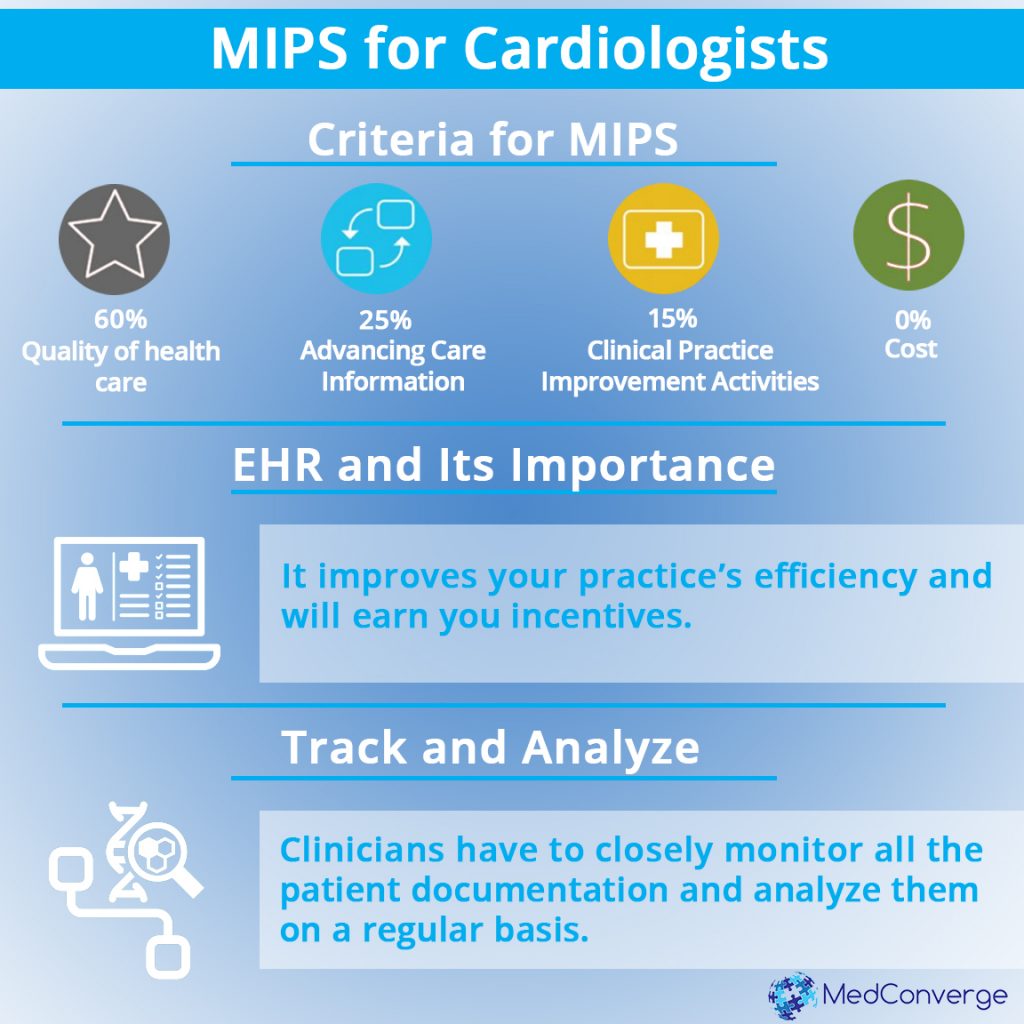
According to MIPS instructions, your Medicare payment adjustment is based on four parameters each with its own weighting. The weighting for the MIPS criteria are as follows:
Quality (60%): it assesses the quality of the medical services rendered to the patient in a timely fashion.
Advancing Care Information (25%): This includes recording all the necessary information about the patient and their illness using a certified electronic health record (EHR) technology.

Improvement Activities (15%): This refers to a variety of patient care facilities such as patient safety, hospital population management, health equity and more meant to improve patients’ lives.
Cost (0% currently, is expected to change in future): This is based on the Medicare claims data, but is not used in the adjustment of the first payment year (CY2019).
If you choose to participate in the Quality Payment Program via MIPS, you can opt for one of three integration options in the first year, namely test, partial and full.
These choices are geared to assist you in understanding how MIPS works for your practice and how you can redesign your billing and data collection process in order to make it easy for you before you integrate it fully into your practice.
Why MIPS Introduction is Important
Total healthcare spending accounts for almost 18% of the American economy. This figure is projected to grow by 5.8% annually for the next decade. As such, it has attracted the attention of budget cutters and politicians.
Medicare and other programs from the federal government cover around half the health expenditures. Medicare covers the healthcare of at least 50 million Americans. Of this budget, cardiac services accounts for 40%.
Medicare payments to hospitals and doctors in the last 50 years enabled the accomplishment of many of the procedures that characterize modern cardiology
What are the examples of these procedures?
They include interventions, imaging, hypertension treatment, surgery, hyperlipidemia and HF.
At the moment, cardiologists and other professional medical organizations are keeping a close eye on the changes in the payment structure for healthcare delivered to Medicare beneficiaries.
Why EHR is Important in MIPS Healthcare
Cardiologists should work closely with their EHR vendors to ensure that their online and digital systems are suitable enough to handle the requirements of the MIPS.
Make sure to choose the six necessary measures that are to be submitted to the MIPS quality category, and understand how these numbers fare against the national benchmarks.
This will give you a clear picture of where you have deficiencies, enabling you to improve on such factors at the earliest.

You can easily have your EHR vendor customize your systems to incorporate these measures. This will ensure that you are recording and filing the right information as and when required.
The reports generated by the EHR have to be taken seriously, and you should work towards improving those numbers to match the national average, at the minimum.
Cardiologists Do Not Understand MIPS and MACRA
Even though the implementation of MACRA may be underway, it is still confusing many in the cardiovascular community.
In one seminar, 29% of the attendees said through the audience-response tool that their practice is yet to become ready for MACRA while 35% said that they had no clue who is responsible for ensuring that MACRA works.
Danger of Cardiologists Not Adhering to MIPS in Their Medical Practice
Even if the financial penalties and incentives aren’t sufficient enough to convince cardiologists to take part in MIPS, there is the likely reputational and long-term impact on their careers.
In the past, primary care physicians would refer patients to specialists and patients would adhere to their directives.
Of the 926,119 active physicians in the US, more than 50% are categorized as specialists. Primary care physicians are accustomed to the reporting requirements of Meaningful Use and the Physician Quality Reporting System.
As such, primary care physicians may only refer their patients to cardiologists who adhere to MIPS, and discourage the patients from visiting cardiologists who do not adhere to MIPS.
Is This Additional Work for Cardiologists? They Are Already on the Brink of Burnout
Many cardiologists report that they are burdened by too many bureaucratic tasks, long working hours and increasing computerization.
This, according to the cardiologists consumes a lot of time that should instead be spent with patients.
And now, they also have to deal with MIPS!
With MIPS, each specialty is benchmarked alongside its peers, meaning that it no longer is about failing or passing. Instead, every tenth of a point translates to a proportional reputational and financial impact.

The MIPS quality performance category contains specialty measure tests, which are groups of measures designed to help specialists in measure selection.
The problem at the moment is that many specialists’ measures lack peer benchmarks.
The lack of benchmarks also applies to many of the measures that are available on the Qualified Clinical Data Registry reporting method, which is increasingly favored by clinicians within their specialty societies.
MIPS Will Affect Cardiology Workflows
The new reporting requirements in quality measures may require substantial changes in cardiology workflows. This will ultimately complicate their already limited choices concerning quality measures.
While cost performance was excluded from MIPS in 2017, it will likely account for 10% of the MIPS score in 2018. Cost performance is mainly centered on episode-based cost measures that gauge the average Part A and Part B Medicare costs.
Cost measures in MIPS medicare are usually centered on procedures initiated and offered by specialists. However, most MIPS quality measures are focused on primary care.
Even though MIPS measures are quite new, cardiologists should assess its impact on their workflows, how they account for cost and, based on the performance feedback from CMS, determine where to make improvements.
Bringing in the Experts Vs Do-It-Yourself
Is there a possibility of cardiologists taking the DIY approach in MIPS?
What determines the answer to this question is the technological sophistication of the practice, the likelihood of risk and the ability to update oneself with the ever-changing regulations.
The CMS has already shown that there will be yearly changes at the very least to the reporting structure and quality measures.

Based on one Health Affairs study, physician practices in the four main specialties spent around 785 hours per physician in an attempt to comply with value-based programs prior to the introduction of MIPS.
CMS understands that there is a lot of complexity involved in integrating MIPS reporting into small practices. As such, it has dedicated $20 million annually for the next 5 years to fund education and training for Medicare clinicians.
On the other hand, physicians in large practices must make a decision on how they will make MIPS reports. For example, they should decide whether or not to report as individuals or as part of a group.
They also need to make a choice on whether or not to restructure a multi-specialty practice or become part of an ACO.
Regardless of the path taken by the specialty practice, there will be long-term reputational and financial repercussions.
By working with an expert in quality reporting, a cardiologist can better understand the significance of each alternative. As you’ll see in the next section, it is important to first decide the measures to report as this will affect the quality score.
Finding the Right Measure to Implement
It is vital to determine the measure improvements that will result in the highest quality score. It is also important to assess what the quality score will look like in different circumstances.
An estimate of the program’s overall financial impact on the organization should be taken. Cardiologists should also predict and keep an eye on their performance relative to the benchmarks.
Finally, it is important to evaluate the reporting method that will produce optimal scores for the organization.
When working with an expert third-party company, cardiologists hire one that is committed to their success and keep reviewing, interpreting and integrating the complex and always changing rules as they are released.
While MIPS inherits most characteristics from PQRS, VBM and Meaningful Use programs, slight differences exist. Therefore, penalty avoidance and high performance does not have the same outcomes under MIPS.
Steps to Choosing Outcome Measures for MIPS
The first step is to select one or more outcome measures. For the MIPS Quality Performance Category, you must report more than one outcome measure.
In case there are no outcome measures applicable to your patient population, then select one or more high-priority measures.
The outcome measure you choose to report is responsible for the six measure requirement for the Quality Performance Category.
If you report more outcome measures beyond the required ones, you will get two bonus points in the QPC score.

The second step is to select an applicable high-priority measure. In case you were able to select an outcome measure, then consider this an optional step.
Remember that measures that are high-priority and are not outcomes earn an extra point in QPC. This makes it a good idea to include as many outcomes and high-priority measures as possible in your six QPC measures.
The final step is to ensure that you have six selected measures. In case you have not yet chosen six measures and are aiming for a positive MIPS payment adjustment, you should choose from other recommended measures.
If you report more than six measures, CMS will compute your MIPS quality performance score using your top performing quality measures.
Importance of record keeping
A cardiologist should occasionally look themselves up on CMS.gov, to check their online reports, and compare their standing with respect to that of their peers.
You should especially keep track of the Quality and Resource Use Reports (QRURs), which includes the readmission rates of the facility.
Also, you should keep track of every patient’s documentation. Digitization of record-keeping has made it easy to record, access and retrieve information.
Use this to your advantage, and update the patient information on a digital sphere with every chance you get.
If you run a cardiology practice and are worried about making sense of the MIPS, fret not.
Our experts at MedConverge will help assist you in all aspects of your billing, thus ensuring that your practice adheres to the necessities put forth by the appropriate authoritative bodies, thus staying in accordance with the MIPS.
For more information on how MedConverge can assist you with your Cardiology Billing, take a look here.
References
- David, K. B. (2017, January 30). MIPS tips for cardiologists feeling clueless about MACRA. Retrieved May 21, 2017, from Cardoivascular Business: http://www.cardiovascularbusiness.com/topics/healthcare-economics/mips-tips-cardiologists-feeling-clueless-about-macra
- Liberman, J. D. (2016, June). MACRA implementation brings radical changes to cardiology practice. Retrieved May 21, 2017, from Healio Cardiology Today: http://www.healio.com/cardiology/practice-management/news/print/cardiology-today/%7Ba1ffca0e-9fcc-48ed-a485-cfcd9312bd3c%7D/macra-implementation-brings-radical-changes-to-cardiology-practice
- N/A. (2017, May 21). Educational Resources. Retrieved from Quality Payment Program: https://qpp.cms.gov/resources/education