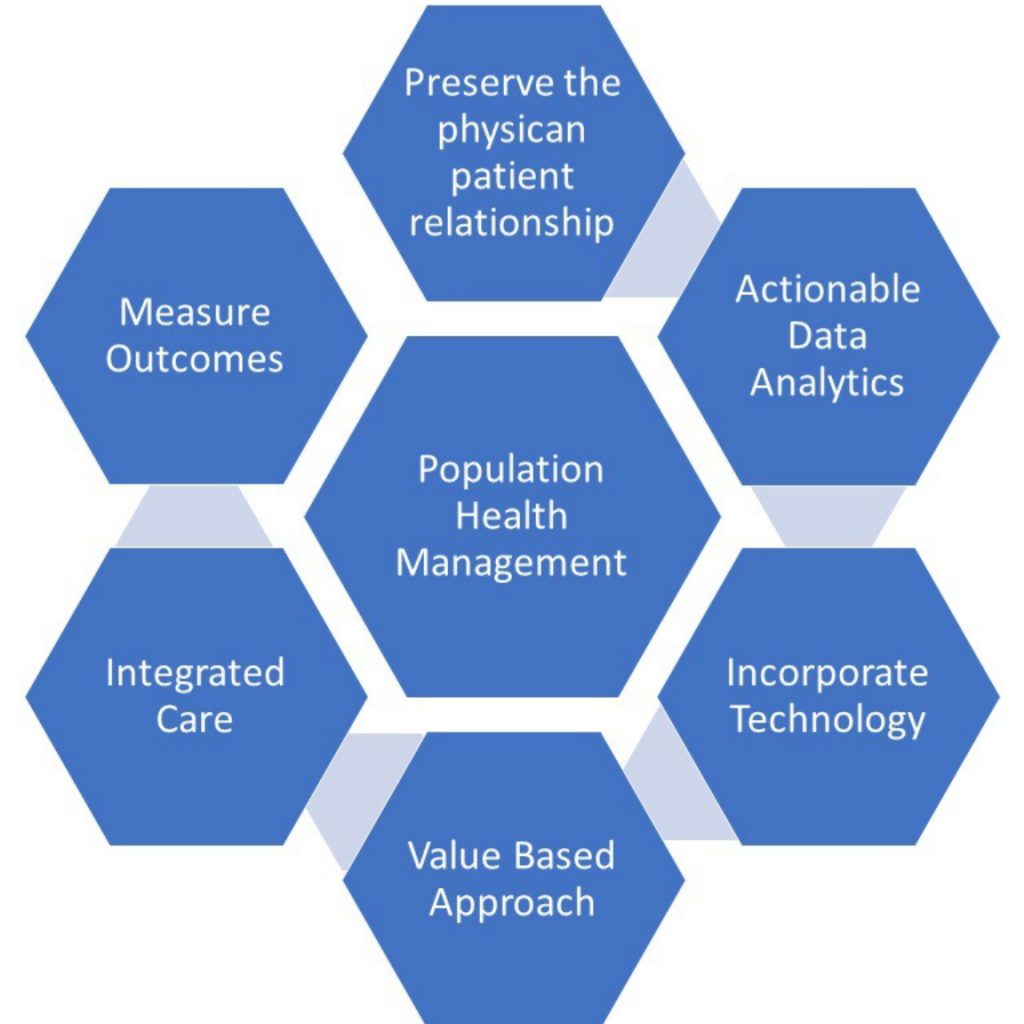
The basic goal of population health management is to manage the health of a defined population optimally by providing the right intervention(s) to the right people at the right time. Well-designed population health tools when implemented thoroughly, benefits the patient, makes workflow easier for the provider and keeps costs low for health systems and payers. However, over time, what has become clear is that the provider must be engaged in the process. At the end of the day, the physician has the relationship that matters most to the patients after their own family, and population health management is about care.
As payers recognize this important influence, they must partner with practices if there is any hope to achieve the PHM aim. Through programs like patient-centered medical homes, payers are attempting to move physicians toward value-based care in an integrated care model. A PCMH requires population health management in order to support incentives and treat patients uniquely based on their specific risk factors. Accountable care organizations are making this work, validating the benefits of value-based care.
Preserve the patient-physician relationship
Population health management isn’t about data and analytics; it’s first and foremost about caring for people. Population health data use should be organized around the patient-physician relationship. In designing for population health management, any new solutions or features need to answer this question first – how does the program support this relationship?
Data and analytics should be useful and actionable
To be truly useful, big data, small data or something in between has to be actionable. Just knowing who is at risk is not enough; there has to be realistic and impactful feedback at the time when patients are willing to hear it. Timing is crucial in PHM.
Technology plus transformation
Transformation that works, combined with the right population health management tools, can double per physician revenue in a fee-for-service or value-based care model. Without hope of a financial incentive, physicians will view population health management the same way they view the introduction of a new electronic health record — more work, less productivity and negative financial consequences.
Think like a payer
Payers and providers manage and analyze data differently. Much of the value-based care model centers on risk sharing between providers and payers. So, the better you can understand the payer’s perspectives and drivers, the more effectively you will be able to negotiate contracts with them. Population health management needs to be designed so that data and reporting help payers and providers work together to get the patient moving in the right care direction.
Shift from treatment to prevention
Healthcare organizations need to embrace the value-based systems that incentivize wellness care over illness treatment. If not, the discrepancies inherent in the fee-for-service model will rapidly eat into profitability.
Think Team; not individuals
Integrated care is an essential component of population health management because special populations require the care of multiple providers who must work together. Organization and reinforcement of “the team culture” must be continual.
Customer service is the key
Healthcare is still figuring out what retailers have for years – customer service is what makes the difference. To be successful, population health management must touch patients through an engagement that delivers on the success of strong customer service management principles.
Measure outcomes
Measure the financial, clinical and experiential impact that your actions are having on your populations. It sounds obvious and elementary, but it must not be discounted as something that an organization will get around to doing later. Payers care about outcomes — and your ability to negotiate gain-sharing contracts will depend on your ability to demonstrate quality of care. Likewise, patients – thinking as consumers – will increasingly want to use these metrics in their own decision-making processes.
There are many facets to a successful population health management strategy. It’s become increasingly clear that organizations need new strategies and tools to effectively care for the risk-based world. A well-designed, thoroughly integrated population health management strategy brings together customer service, clinical decision support and the right data to build something revolutionary in healthcare: better outcomes.
References
- (2016 , February 02). Population health management 101: New strategies and tools to care for high-risk patients. Retrieved Septemeber 25, 2017, from http://www.healthcareitnews.com: http://www.healthcareitnews.com/news/population-health-management-101-new-strategies-and-tools-care-high-risk-patients
- Navigate population health. (2017). Retrieved September 25, 2017, from www.athenahealth.com: https://www.athenahealth.com/knowledge-hub/population-health/strategies
- Population Health Management: Systems and Success. (2017). Retrieved September 25, 2017, from www.healthcatalyst.com: https://www.healthcatalyst.com/population-health/
- Population Health Management: What’s Your Strategy? (2017). Retrieved September 25, 2017, from www.hsgadvisors.com: http://hsgadvisors.com/thought-leadership/articles/population-health-management-whats-your-strategy/