Revenue cycle is defined by the Healthcare Financial Management Association as “All administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” The term includes the entire tenure of a patient account – from its creation to the payment. The process of revenue cycle flows into and affects each component of the system. Executed correctly, the revenue cycle performs as predicted; but, any problem early in the cycle can and generally does have significant ripple effects. The longer and further an error travels through the system, revenue recovery becomes that much more costly.
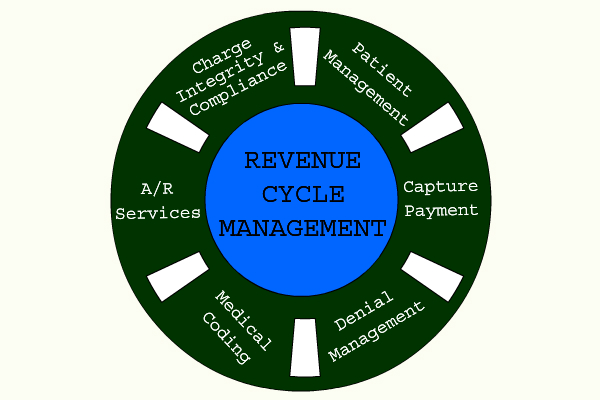
Revenue Cycle Management (RCM)
The new buzzword in the healthcare industry, revenue cycle management services are now being offered by a large number of companies to healthcare providers. In order to make a decision whether your organization requires these services, it is important to understand what revenue cycle management is all about. To a lot of healthcare providers, RCM means performing the basic medical billing functions like filing claims, working rejections and billing patients. However, there is a lot more to RCM than just that.
The cycle starts with the patient making an appointment, and ends when the account balance for that patient stands at zero. In order to achieve the maximum revenue, the first step is to understand the revenue cycle in its entirety. Achieving maximum revenue does not mean overcharging the patient or manipulating the accounts; it simply means that you are smarter about the services you provide and getting the payment for them with the least amount of efforts and costs involved. It is important to remember that while the first priority of any healthcare system is to provide care for the patient, neglecting the revenue cycle may soon create a situation where the healthcare provider would no longer be in a position to provide services due to mounting losses.
Who and what affects RCM in your organization?
Traditionally, the billing office has always been looked at as a ‘back office’ function; meaning that the revenue cycle starts after the patient leaves the clinic. However, a closer look at the revenue cycle will show that it actually begins with the patient walking into the clinic and every member of your clinic affects your ability to be paid in full. Let us look at the role of a few key people in the revenue cycle:
- The person scheduling the appointment has to remind the patient that a co-payee is expected when they come to the clinic. It is also important that the person checks the patient’s previous records and collects any outstanding dues.
- When checking in the patient, the person responsible has to ensure that the dues for the current visit is collected, while accurately capturing insurance information and making the patient understand the coverage.
- The clinician has to get an Advance Beneficiary Note (ABN) waiver signed, make sure that the documenting and coding are done correctly.
Every person in the clinic is responsible for the revenue cycle. In order to effectively manage your revenue cycle, you have to train each member of your organization to understand how their role affects the revenue cycle and implement their roles as a standard procedure. Instead of hiring people to work rejections and passing financial matters to the back office, ensure that every person in the clinic works with the process and thus prevents rejection in the first place itself. Collaboration and understanding across the clinic facilitates will definitely maximum revenue for your practice.
How to optimize your revenue cycle
Here are some pointers that will help you optimize your revenue cycle management process:
- Ensure that each member of your clinic understands how their job impacts the overall revenue – you could ask them to write a small note about their job and its impact on the cycle. Analyze the rejections and denials as this will give you an understanding of areas where the clinic needs to improve. Share the analysis with all members of the staff and clearly define their roles and expectations. Work out a program to measure their effectiveness and ask them to provide regular feedbacks.
- Use technology to its fullest. The practice management / EHR system should help in providing you with tools that automate processes. Make sure that the vendor understands your workflow and provides the right tools for the same.
- Ensure that you have the correct person as your Revenue Cycle manager. This is a critical position and needs a competent person to handle it.
Outsourcing your Revenue Cycle Management
In case you feel that you either do not have in-house talent to handle your revenue cycle management, or it is not cost effective to do so internally, you can outsource parts or all of these services to an outside party. However, the key once again is to finding the right outsourcing company for your clinic. So, how do you find the right partner for your RCM?
- Does your PM / EHR vendor offer these services? If yes, they are in the best position to ensure the processes in the clinic occur efficiently.
- Ensure that the outsourcing agency allows full visibility into what they are doing. You should also continue to own your data. You will also need to work with your outsourcing vendor to understand the key metrics.
- Find the right vendor who will not only perform the necessary functions relating to billing and work rejections, but will also provide you with feedback and tools to prevent future rejections. They should also work with you to train the staff and help implement best practices in your clinic.
As the healthcare landscape changes, it is critical you have the right team in place to care for your patients and your practice. Contact us at info@medconverge.com for any queries regarding RCM that you may have.