One of the most important considerations during the medical billing and coding process is to choose whether the patient is an inpatient or an outpatient. Based on the choice, the medical codes associated differ.
At times, inexperienced medical coders may unintentionally misrepresent the patient status which could result in denied claims and even accusations of fraud. What’s the difference between inpatient and outpatient coding?
By the end of this article, you will know the difference between inpatient and outpatient services.
What is inpatient?
An inpatient is an individual who has been officially admitted to the hospital under a physician’s order. The patient will remain classified as an inpatient until one day before discharge.
Look:
Staying in the hospital overnight does not necessarily mean that the patient is considered an inpatient.

Inpatient Medical Coding
Inpatient coding is related to the patient’s extended stay service. Examples of Inpatient facilities include acute and long-term care hospitals, skilled nursing facilities, hospices, and home health services.
Here’s why this matters:
During the stay, the patient may have a variety of tests run, will have changes in diagnosis and treatments. A lengthy stay usually results in extensive and intricate patient records which makes it important to have an experienced medical inpatient coder doing the job.
So what is outpatient care, who is an outpatient and what is outpatient services?
Outpatient
A patient that comes to the ER or practice, and is being treated or undergoing tests, but has not been admitted is considered an outpatient, even if the patient spends the night.
Outpatient Medical Coding
Outpatient coding focuses on the direct treatment offered in a single visit, which is usually a few hours. A basic rule of thumb is that outpatient care has a duration of 24 hours or less.
With the increased development in the medical field, many services that used to be considered inpatient treatments are being assigned to outpatient services.
Payments
Original Medicare inpatient claims are paid under Part A, whereas outpatient claims are paid under Medicare Part B.
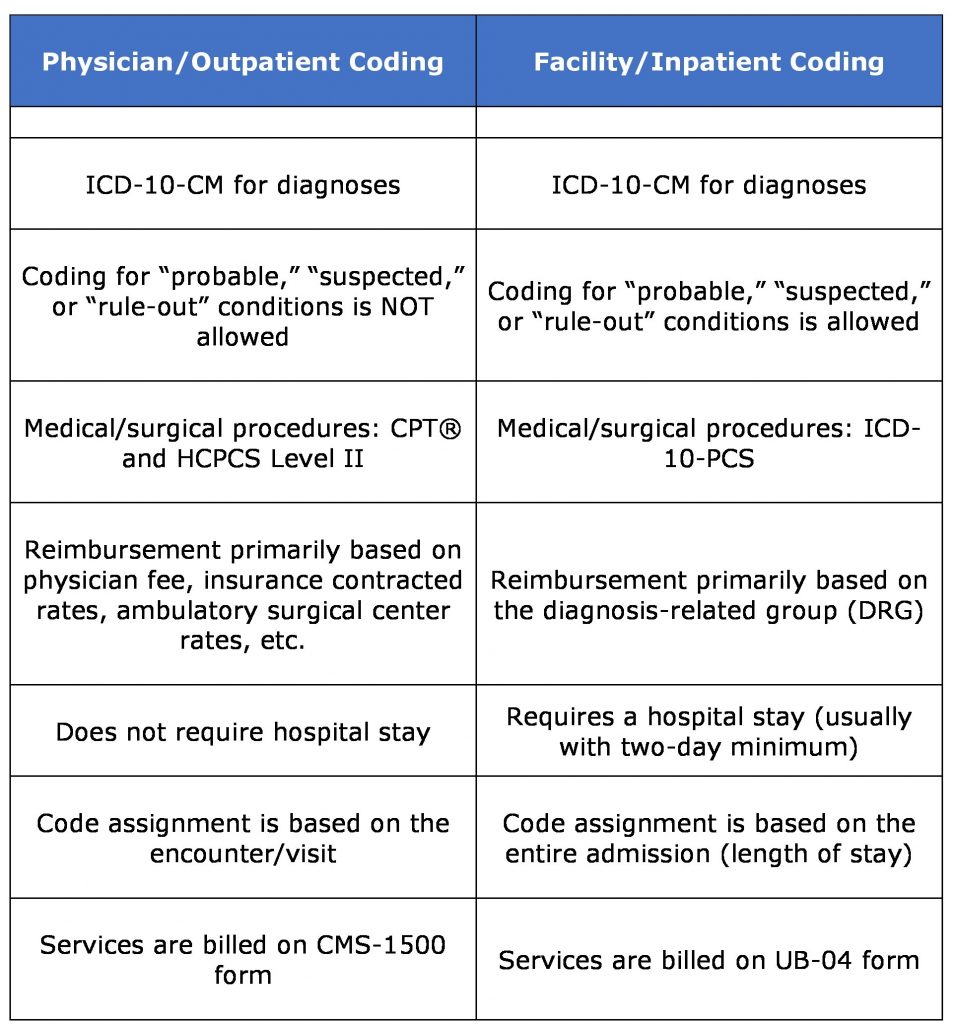
Inpatient medical coding is reported using ICD-10-CM and ICD-10-PCS codes, which results in payments based on Medicare Severity-Diagnosis Related Groups (MS-DRGs). Outpatient medical coding requires ICD-10-CM and CPT®/HCPCS Level II codes to report health services and supplies.
Examples of Medicare Part B services include hospital care, emergency department services, lab tests, X-rays, outpatient surgeries, and doctors’ office visits.
Diagnosis
In an inpatient facility, medical coders must determine the principle diagnosis for the admission, as well as present on admission (POA) indicators on all diagnoses.
Diagnoses listed as “probable,” “suspected,” “likely,” “questionable,” and other such terms, may be coded when documented as existing at the time of discharge and no definitive diagnosis has been established.
The diagnostic workup, arrangement for further workup or observation, etc. needs to relate to the established diagnosis.
That’s not all…
A common mistake is to code uncertain diagnoses that are not documented at the time of discharge/on the discharge summary – do not do that as they may have been ruled out during the stay.
An example of an uncertain diagnosis is ‘Appears to be’ while ‘evidence of’ is not considered an uncertain diagnosis.

Difference Between Inpatient and Outpatient Coding (Inpatient vs Outpatient)
In comparison, for Outpatient medical coding, coding for uncertain conditions is not allowed. The following table shows the difference between inpatient and outpatient treatment.
An overview of Inpatient and Outpatient Coding:
Conclusion
No matter what the situation, medical coders need to keep abreast of the changing regulations along with inpatient coding guidelines and outpatient coding guidelines with respect to medical billing. The hospital facility may have its own set of standard protocols that need to be followed.
One may say that outpatient coding is less complex compared to inpatient coding – but that does not necessarily mean that it’s any easier.
Experience, knowledgeable and certified coders specific to outpatient and inpatient coding can be the difference between a denied claim and receiving the reimbursements you deserve.
If anyone ever asks you “what is the difference between inpatient and outpatient,” you now know how to answer them.
Since you clearly understand the difference between inpatient and outpatient care get in touch with us if you’d like to know more or need assistance with your medical billing and coding.
Also, let us know in the comments section below whether this article was helpful. Did the article change what you initially thought was the difference between inpatient and outpatient coding?
References:
- https://www.aapc.com/blog/40261-inpatient-and-outpatient-coding-call-for-distinct-codes-and-guidelines/
- https://www.cms.gov/Medicare/Coding/ICD10/Downloads/2018-ICD-10-CM-Coding-Guidelines.pdf
- https://www.aapc.com/blog/40261-inpatient-and-outpatient-coding-call-for-distinct-codes-and-guidelines/
- https://www.aapc.com/blog/31321-is-your-next-step-inpatient-coding/
- https://libmaneducation.com/comparison-of-inpatient-outpatient-coding-right/
- http://mmiclasses.com/inpatient-vs-outpatient-coding/
- http://medical-coding-carers.blogspot.com/2010/05/inpatient-coding-vs-outpatient-coding.html
- http://slideplayer.com/slide/13023570/